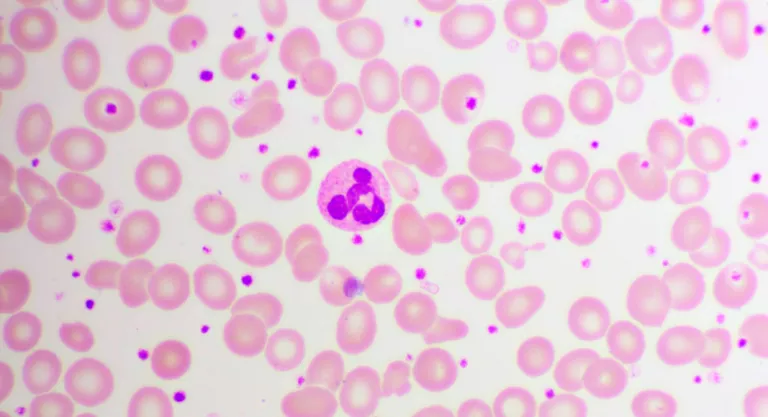
Platelets – also called thrombocytes – are blood cells produced by the bone marrow and that are involved in the formation of blood clots to prevent, for example, bleeding from bleeding when we cut or wound ourselves, since platelets join and plug blood vessels to decrease bleeding. It is important that your levels are adequate – not too low, not too high – because otherwise health problems appear.
Thus, when a person has too low platelets, they can suffer from thrombocytopenia, which makes them prone to bleeding and bruising. If, on the other hand, the body produces too many platelets and has a high level of platelets in the blood – known as thrombocytosis, thrombocythemia or hyperplateletosis – it could indicate that it lacks iron – as occurs in iron deficiency anemia – or that you have an infection or inflammation, but it can also alert you to the development of cancer.
“Thrombocytosis is an increase in the number of platelets in the blood” explains Dr. Manuel Pérez Encinas, member of the Spanish Group for Negative Philadelphia Chronic Myeloproliferative Diseases (GEMFIN), of the Spanish Society of Hematology and Hemotherapy (SEHH) and hematologist at the Clinical Hospital of Santiago de Compostela. “Thrombocytosis is usually a reactive phenomenon, since it behaves like an analytical datum called an acute phase reactant. Other acute phase reactants are increased leukocytes, increased C-reactive protein, or increased ESR. The platelet count can increase nonspecifically in many clinical situations where there is an inflammatory component.”
There are two types of thrombocytosis:
Why do blood platelet levels increase?
In a blood test you can see if the number of platelets is correct. This must range between 150,000 and 400,000 mm3. Blood platelets are considered high when their count is 400,000 mm3 or higher.
“Only when the values are in very extreme ranges, such as more than 1.5 million platelets or more, can symptoms related to this alteration occur: bleeding or hemorrhage can be triggered, and also thrombosis at the level of the arteries” , indicates Dr. Javier Anguita, Head of the Hematology and Hemotherapy Service Section at the Hospital General Universitario Gregorio Marañón, in Madrid.

“Any pathology with an inflammatory component can cause thrombocytosis. This includes, for example, an infection, trauma, arthritis, colitis, some tumors with an inflammatory component, etc. The list is endless and the clinical history is the key to guide the diagnosis”, explains Dr. Pérez Encinas, member of GEMFIN. In other words, reactive thrombosis is a symptom of another disease, which according to these experts can be:
What type of cancer can increase platelets?
Dr. Pérez Encinas indicates that “a minority of cases of thrombocytosis are due to blood tumor diseases called myeloproliferative neoplasms”, and those that cause thrombocytosis, according to this hematologist, are above all polycythemia vera, myelofibrosis, or leukemia chronic myeloid. In this case, he adds, “diagnosis is made with a blood count, a bone marrow biopsy and mutation studies, such as JAK2V617F, CALR and BCR-ABL mutations.” In the blood count, he points out, in addition to the increase in platelets there are also other alterations, such as an increase in leukocytes, or an increase or decrease in hemoglobin.
“It is exceptional that a solid tumor is diagnosed only by high platelets, but in the event of thrombocytosis, a complete study is carried out to rule out its most frequent causes, including tumors”
Dr. Javier Anguita points out: “Any tumor can have a secondary high platelet count. The most frequent are those of the breast, colon, prostate, lung and ovary. In general, the symptoms of the tumor appear before or at the same time as the high platelets and it is rare that a solid tumor is diagnosed only by the high platelets; however, in the event of thrombocytosis, a complete study is carried out to rule out the most frequent causes of reactive or secondary thrombocytosis, including tumors”.
Symptoms of thrombocytosis or high platelets
People with reactive or secondary thrombocytosis usually do not show symptoms, and those they experience are related to the disease that has caused this alteration, so it is usually detected when the patient has a blood test that is part of an examination routine health, or other reason. The important thing, according to Dr. Pérez Encinas, is to study the cause for which the thrombocytosis has appeared.
In the case of people with essential thrombocytosis, they may present symptoms related to the presence of bleeding or blood clots, such as:
In cases of tumor thrombocytosis due to myeloproliferative neoplasia “vascular symptoms may appear. The usual ones are the so-called microcirculatory symptoms due to obstruction of the blood circulation in the small vessels”, such as:
How to control thrombocytosis and lower platelets
The treatment of thrombocytosis varies depending on whether it is reactive or essential:
Treatment of reactive thrombocytosis
When the health problem that has caused the increase in platelets is resolved, their levels return to normal. Dr. Pérez Encinas tells us that reactive thrombocytosis is not treated because it does not usually cause symptoms, and that “what needs to be done is to identify and treat the cause of thrombocytosis.” Therefore, “in secondary disorders, thrombocytosis is associated with the treatment and evolution of the underlying disease. The thrombocytosis will disappear with the treatment of the disease”, explains the Head of the Gregorio Marañón Hematology and Hemotherapy Service Section. For example:
In the case of reactive or secondary thrombocytosis, if it has occurred because the individual has lost a lot of blood following trauma or recent surgery, the platelet levels return to normal on their own when they recover from their injuries.
If it is due to an infection or inflammatory disease, the platelet count will remain elevated until the underlying disease is well controlled medically.
In people with the spleen removed by splenectomy, their blood tests could always reflect thrombocytosis, but it would not require treatment to solve it.
Treatment of essential thrombocytosis
In primary cases, that is, essential thrombocythemia, “we will have to do a long-term follow-up, since there is no curative treatment at the present time. In cases in which the risk of thrombotic or hemorrhagic complications is high, treatment with a cytoreductive drug will be established. A mild cytotoxic effect to lower the number of platelets and other blood cells that may be elevated. If any thrombotic complication has occurred, it will be treated with an anticoagulant or antiaggregant, depending on the thrombosis”, indicates Dr. Anguita.
For Dr. Pérez Encinas, “thrombocytosis associated with myeloproliferative neoplasms should be treated, as they can cause thrombotic and other symptoms as they are tumors. Each entity has a specific management, and the management of essential thrombocythemia is based on the control of cardiovascular risk factors, antiaggregation (generally acetylsalicylic acid) and cytoreductive drugs to reduce the number of platelets.
.